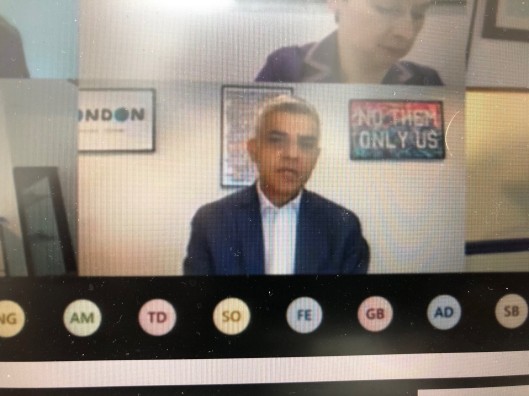
Sadiq Khan (above) was asked at Mayor’s Question Time yesterday about his recent comments (to The Sunday Times Magazine) on his own mental health during the coronavirus pandemic.
A summary of his remarks to the London Assembly yesterday are reported today in the Evening Standard.
Below is a fuller transcript of what he said verbally, during the “virtual” MQT meeting, in response to the written question below from Tony Devenish, a Tory member of the London Assembly.
Mr Devenish’s question (London Leadership Question No: 2020/2518) had been submitted in advance and selected for a verbal response from the Mayor.
Mr Devenish asked: “On 21st June 2020 you told the Sunday Times that you had ‘not been providing proper leadership’ as Mayor of London. While you have our sympathies, do you not think you should have notified the London Assembly and shared this with the GLA Leadership and Londoners?”
The Mayor introduced his remarks to MQT by saying he wanted to set an example by being “open and honest” about his own mental health, as it may encourage others to seek support.
He has previously spoken to the Evening Standard and others about his mental health.
Mr Khan said: “None of us are superhuman. We all have our good days and our bad days. This is especially true in the middle of a pandemic, when we are all finding it tough and we are all being asked to make huge sacrifices to help save lives, from staying indoors and working at home, to limiting outdoor exercise and our interactions with friends, family members and loved ones.
“I make no apology for acknowledging the toll lockdown has had on Londoners’ mental health, including my own.
“It would be irresponsible and dishonest to pretend this period has been easy for people living in our city.
“I’m pleased to say that many Londoners, including City Hall staff as well, have thanked me for speaking so openly about this issue, and I will continue to do so….”
He said he had no desire to be seen as “some sort of Alpha male who constantly seeks to parade their virility”.
He continued: “We are all human. We all have days where we are not firing on all cylinders, as I’m sure even Assembly Member Devenish can confirm.
“But I can say with confidence, I don’t think there has been a single day during this crisis when this administration, and my team, hasn’t provided the leadership that London needs.”
Mr Devenish: “This is the biggest crisis our country has faced since World War Two, and you tell the Sunday Times what you said. You didn’t tell the London Assembly. Why was that?”
The Mayor: “I’m quite surprised at this question because all of us will have days or periods where we have physical ill health. We will all have periods where we could have family bereavement or other issues. Similarly we will have issues when we are not 100 per cent. There has been no criticism in the past in relation to those, which is human nature.
“There appears to be a criticism of me based on me being honest about how I’m feeling…. This is one of the reasons there is stigma around mental health and people talking about mental health.
“One of my roles as a politician is to follow the advice of the previous Prime Minister, which is to use our role to educate people. I’m not hesitating in my role to talk about mental health, in relation to how I feel.
“The reality is that I have not taken time off because I have not needed to… talking about it can be a big way of addressing this. I’m not sure what the criticism is: that I should be sharing with the assembly every day I’m feeling a bit poorly?
“The reality that me talking about it has encouraged others to talk about it, and I will continue to do so, even if it continues to lead to criticism from Conservatives.”
Mr Devenish: “Just for clarity, Mr Mayor, I’m not criticising you for having the guts to talk about it. I’m congratulating you. What I am asking you: that during the largest crisis since World War Two, that you would actually inform the assembly rather than the Sunday Times in a piece which, frankly many people have approached me and said they were amazed at the way you broached the subject. It’s the way you have done it, not the fact that you have done it. Can I finally ask you: do you not feel that if you were clearly unwell at times, you should have stood down temporarily, put your deputy mayor in charge and informed the assembly?”
The Mayor: “What you don’t understand is that your question illustrates one of the reasons why people are scared to talk about their mental health. You assume that it automatically makes someone unfit to do the job that they are doing. That is one of the reasons why people in places of work across our city, and across our country, don’t talk about it with their line managers or their other colleagues, because people like you say that means you are unfit to work. All of us have periods where we are not firing on all cylinders. All of us, if we are honest, are not always at 100 per cent. I will not stop being honest with Londoners about the fact that we should talk about mental ill health.
“My age cohort, men aged 25 to 49, are the largest group of people who, I’m afraid, kill themselves because of mental ill health. The sort of attitude that leads to the question being asked, leads to men not having the confidence to do so. Three-quarters of people who kill themselves are men, so me talking about it – albeit, there are people who criticise me – I’m going to carry on doing so.”
Mr Devenish: “By the way, Mr Mayor, I didn’t criticise you. I asked a question. Thank you.”















